- Understanding Evidence-Based Clinical Reasoning
- The Impact of AI on Evidence-Based Clinical Reasoning
- Challenges and Considerations in AI-Enabled Evidence-Based Clinical Reasoning
- The Evidence Base for AI-Driven Healthcare
- The Importance of Continuous Learning and Adaptation in AI Development
- Partner with Softarex for Cutting-Edge Solutions
In recent years, the healthcare industry has undergone a remarkable transformation with the emergence of AI-enabled products. This shift has been further reinforced by the projected growth of the healthcare AI market, which is expected to reach $187.95 billion by 2030. This rapid adoption of AI technologies has impacted various domains of healthcare, including diagnostics, chronic care management, care delivery, triage and diagnosis, self-care, prevention, wellness, and clinical decision support.
To deepen your understanding of AI technologies in healthcare, check out our previous articles here and here.
Evidence-based clinical reasoning is the bedrock of informed decision-making in healthcare. It bridges the gap between cutting-edge AI technologies and the delivery of high-quality, patient-centered care. By integrating the best available evidence, clinical expertise, and patient preferences, healthcare professionals can ensure that AI-driven solutions are not only innovative but also effective, safe, and tailored to individual patients.
Understanding Evidence-Based Clinical Reasoning
Evidence-based medicine plays a crucial role in healthcare by promoting the use of high-quality research evidence to inform medical practices. It emphasizes the importance of critically appraising and applying scientific evidence in clinical decision-making, aiming to improve patient outcomes and optimize healthcare interventions.
In the context of AI-enabled products, evidence-based clinical reasoning is of paramount importance as it enhances their reliability and trustworthiness. These products leverage artificial intelligence to assist healthcare professionals in decision-making processes. By incorporating evidence-based clinical reasoning, AI-enabled products can effectively analyze vast amounts of medical data, identify patterns, and provide evidence-based recommendations to support clinical practice. This integration helps ensure that AI-driven solutions align with established best practices and reliable scientific evidence.
The Impact of AI on Evidence-Based Clinical Reasoning
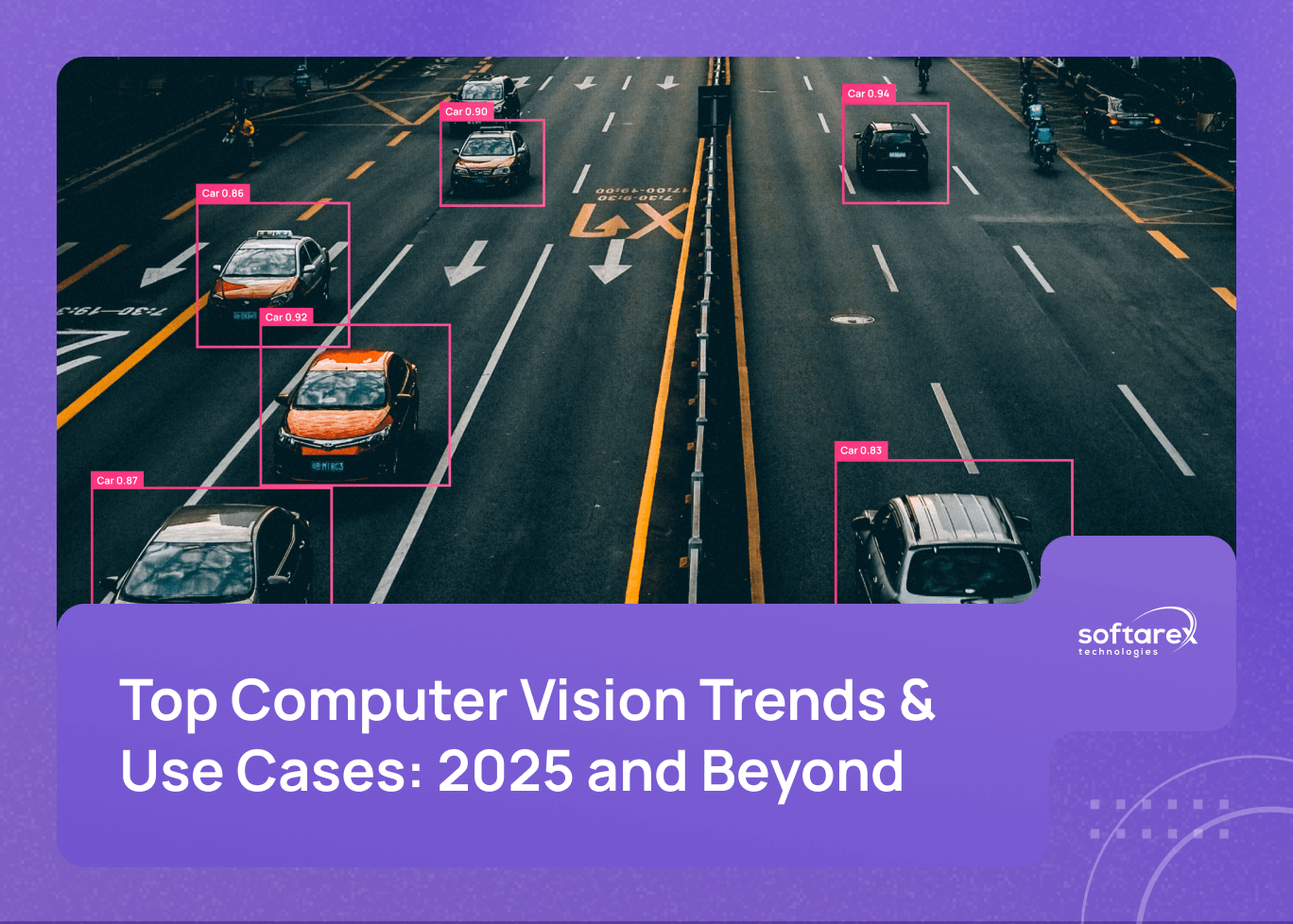
AI technologies provide valuable tools for data analysis and interpretation, significantly enhancing evidence-based clinical reasoning. Through advanced algorithms, AI can efficiently process large volumes of healthcare data, including medical records, research studies, and patient information. This capability enables healthcare professionals to extract meaningful insights, identify patterns, and make evidence-based decisions based on comprehensive and up-to-date information.
This shift towards intelligent, data-driven decision-making is not just theoretical; projects such as our Healthcare Predictive Analytics Tool show how machine learning can actively help clinicians to anticipate patient needs before critical symptoms appear.
Similarly, our Automatic Reflex Diagnostics System shows how AI-powered pattern recognition can transform traditional diagnostic processes. This innovative solution uses computer technology to identify patterns in reflex data that indicate disease, enabling physicians to detect probable pathologies of internal organs and systems at the earliest possible stage — all within 15–20 minutes, compared to the days or weeks required by conventional diagnostic methods.
Machine learning algorithms can help healthcare professionals to synthesize evidence from multiple sources and domains, such as randomized controlled trials, systematic reviews, meta-analyses, guidelines, and expert opinions. By applying techniques such as classification, clustering, regression, and recommendation, machine learning algorithms can aggregate, filter, rank, and summarize the evidence according to its quality, relevance, and applicability. For example, machine learning algorithms can be used to generate evidence summaries or maps that highlight the key findings and gaps in the literature.
AI-powered decision support systems further contribute to evidence-based practice by providing clinicians with real-time recommendations based on the integration of patient-specific data and the latest evidence. These systems can use techniques such as rule-based systems, case-based reasoning, neural networks, and reinforcement learning to model the clinical problem, generate possible solutions, evaluate the outcomes, and provide feedback. For example, AI-powered decision support systems can be used to suggest diagnosis options, treatment plans, or referral pathways based on the patient’s characteristics, preferences, and history.
Challenges and Considerations in AI-Enabled Evidence-Based Clinical Reasoning
We can see that AI-enabled evidence-based clinical reasoning is a promising approach to improve the quality and efficiency of healthcare delivery. However, it also poses several challenges and considerations that need to be addressed.
Data Quality and Integrity
Ensuring data quality and integrity in AI-driven healthcare is crucial, as the performance and reliability of AI models depend on the accuracy and completeness of the data they are trained and tested on. Data quality issues such as missing values, outliers, noise, bias, and inconsistency can affect the validity and generalizability of AI results. Therefore, data collection, preprocessing, and validation methods need to be rigorous and transparent.
Ethical Considerations
Ethical considerations in utilizing AI for clinical decision-making are also important, as AI can have significant impacts on patients’ health outcomes, privacy, autonomy, and dignity. Ethical principles such as beneficence, non-maleficence, justice, and respect for persons need to be upheld when designing, deploying, and evaluating AI systems in healthcare. Moreover, ethical issues such as informed consent, accountability, explainability, fairness, and trustworthiness need to be addressed to ensure that AI is used in a responsible and respectful manner.
Bias in the Data
AI systems can inherit or amplify bias from the data they are trained on, the algorithms they use, or the human decisions they influence. Bias can lead to inaccurate or unfair outcomes for certain groups of patients or populations, such as underrepresented minorities, women, or rural communities.
Right Balance
Balancing AI recommendations with healthcare professionals’ expertise is another challenge and consideration in AI-enabled evidence-based clinical reasoning. AI can provide valuable insights and suggestions based on large-scale data analysis and complex algorithms, but it cannot replace the human judgment and experience of healthcare professionals. Therefore, AI should be seen as a complementary tool rather than a substitute for human expertise. Healthcare professionals need to be able to understand, interpret, and evaluate AI outputs, as well as to communicate them effectively to patients and other stakeholders. Furthermore, healthcare professionals need to be involved in the development and governance of AI systems to ensure that they are aligned with their needs and expectations.
The Evidence Base for AI-Driven Healthcare
A crucial aspect of evidence-based clinical reasoning is the evidence base for AI-driven healthcare. It encompasses diverse sources and types of evidence that inform the design, development, evaluation, and implementation of AI systems in healthcare settings. These sources include research studies, clinical guidelines, expert opinions, patient references, and contextual factors.
To ensure that AI systems are built upon a solid evidence base, developers and healthcare professionals employ appraisal and synthesis tools. PICO (Population, Intervention, Comparison, Outcome) helps formulate clear and focused questions for selecting relevant evidence for specific clinical problems. GRADE (Grading of Recommendations Assessment, Development, and Evaluation) provides a structured framework for assessing evidence quality, considering factors such as study design, risk of bias, consistency, and precision. CAT (Critically Appraised Topic) assists in evaluating the quality and applicability of research findings for AI system development and implementation.
Additionally, reputable organizations offer guidance and frameworks to evaluate the effectiveness, efficiency, equity, and acceptability of AI applications in healthcare. The World Health Organization (WHO) has issued ethics and governance guidance for AI in health, outlining six guiding principles for the design and use of AI in health. The National Institute for Health and Care Excellence (NICE) has developed the evidence standards framework for digital health technologies, including AI, which provides criteria for assessing evidence quality.
The Importance of Continuous Learning and Adaptation in AI Development
AI systems in health care need to be continuously updated and refined to keep up with the dynamic and complex nature of the domain. New data, evidence, guidelines, and technologies may affect the performance or relevance of AI systems over time. Therefore, feedback mechanisms and evaluation methods are essential to monitor and improve the quality and impact of AI systems. Moreover, healthcare professionals and AI engineers need to engage in ongoing learning and adaptation to ensure that AI systems reflect the diversity and needs of different healthcare settings and stakeholders. This includes providing education and training on digital skills, community engagement, and evidence-based clinical reasoning for healthcare workers who may interact with or be affected by AI systems. Continuous learning and adaptation are vital for developing effective and responsible AI-enabled products for health care.
Partner with Softarex for Cutting-Edge Solutions
AI in healthcare has the opportunity to transform the way we diagnose, treat and prevent diseases. At Softarex, we are dedicated to inspiring collaboration, fostering innovation, and promoting the responsible adoption of AI in evidence-based clinical practice. We invite you to contact us today for more information and join us on this exciting journey.
For more in-depth insights into how artificial intelligence is transforming healthcare delivery and pharmaceutical innovation, download our comprehensive eBook, The AI Revolution in Healthcare and Pharmaceuticals. This resource explores cutting-edge applications, real-world case studies, and future trends that are shaping the industry’s digital transformation.