We’ve already explored the benefits of EHR and Meaningful Use — improved quality of care, fast exchange of medical data between providers, reduced risk of medical error, and more. But despite all of them some providers and patients still feel rather skeptical about the idea of migrating medical records into an electronic system. Probably the major concern is the security and privacy of health information. And there’s a good reason for that. According to the HIPAA Journal, there were 3,054 healthcare data security breaches involving over 500 records between 2009 and 2019. Moreover, the number is constantly increasing — 2019 has seen three times more incidents than 2017.
The importance of security in EHR

In the age of digital healthcare, medical records security should be a top priority for all EHR-adopters. Data breaches can have serious implications for both providers and patients.
As for providers, healthcare data security violations negatively affect their reputation, harm the patients, and cause financial losses.
Healthcare data breaches cost providers an average of $6.45 million.
Trust, especially in something so people-centered as healthcare, is an issue of paramount importance. Patients need to be sure their personal information is secure.
The feeling that their data can be stolen and sold on the black market can abuse their trust in the EHR system and physicians. Patients can refuse to disclose their health information, which may have life-threatening consequences.
HIPAA
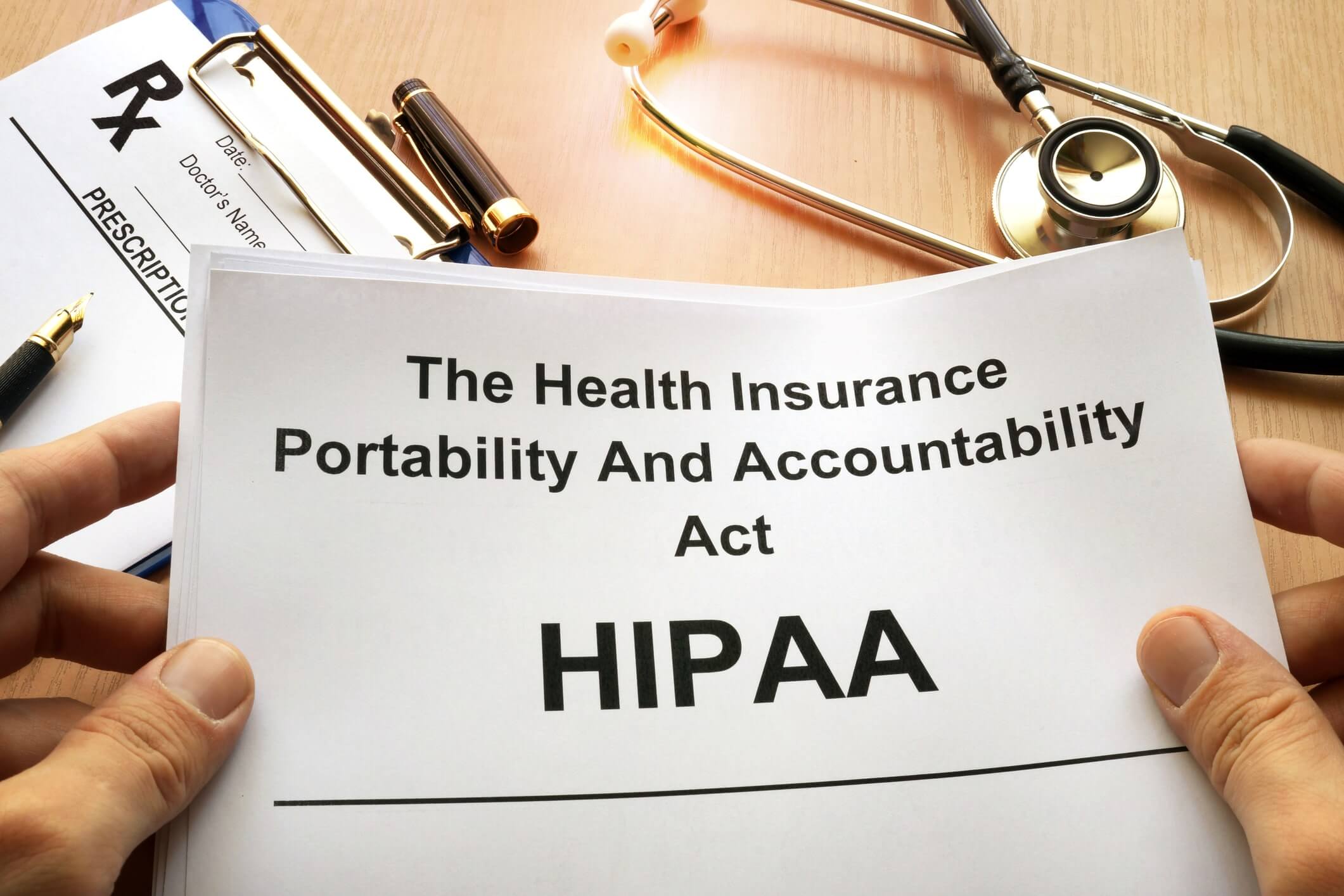
To legally ensure the safety of medical data the US federal government passed the Health Insurance Portability and Accountability Act (HIPAA) of 1996. It requires setting national standards to safeguard patient health information from disclosure via fraud and theft.
HIPAA is a suite of regulations that consists of three main rules:
- The Privacy Rule protects the privacy of personal health information, sets limits and conditions on its use and disclosure, and gives patients rights over their medical information.
- The Breach Notification Rule requires healthcare providers to notify patients of data security breaches.
- The Security Rule establishes national standards to protect the security of individuals’ electronic Protected Information (ePHI). Its aim is to safeguard a subset of information covered by the Privacy Rule.
EHR systems are subject to the HIPAA Security Rule. According to this rule, EHR-adopters should make sure their EHR software possesses the following:
- ePHI encryption. When encrypted health data will be available exclusively to the authorized people.
- Auditing functions. An electronic audit trail will provide valuable insight into the ePHI access history. Simply put, it will help determine what employees have accessed an ePHI, what changes have been made, and when.
- Password protection. A password should consist of alpha-numeric, capitalized, and special characters. Strong passwords will help limit access to an ePHI to authorized users only.
HIPAA Security Risk Analysis
Ensuring privacy and security protection for patients’ personal health information is one of the five main objectives of Meaningful Use and, accordingly, one of the core requirements of the current Promoting Interoperability Programs. Under the HIPAA Security Rule, all healthcare providers participating in the Program must conduct or review a security risk analysis.
According to the HIP Guidance on Risk Analysis, risk analysis is “an accurate and thorough assessment of the potential risks and vulnerabilities to the confidentiality, integrity, and availability of electronic protected health information held by the organization”.
To make it easier for healthcare providers to conduct the analysis, the Office of the National Coordinator for Health Information Technology (ONC and the HHS Office for Civil Rights (OCR) developed a comprehensive and downloadable Security Risk Assessment Tool (SRA Tool). The Tool guides providers through each HIPAA requirement and asks questions about the organization’s activities.
Replying to the questionnaire — there are a total of 156 questions — can help a provider identify potential risks to protected health information. Thanks to that, a provider can timely handle all the issues, for example, carry out staff training in case of password sharing. Therefore, the risk assessment can help healthcare providers avoid data breaches and, thus, improve data security.
EHR security begins with you

Today’s EHR software solutions have all necessary built-in electronic health records security features. However, responsibility for compliance with the HIPAA Security Rule requirements still lies with the providers themselves. No matter how advanced a system is, it can’t ensure the safety of data unless it’s properly used.
In case you feel doubts about your medical data security or need assistance with your EHR implementation, feel free to write to us. Our consultants will gladly guide you on HIPAA compliance and your custom software development.