What is AI?
Artificial intelligence (AI) is a type of technology that simulates human intelligence processes by machines and has the ability to perceive, reason, discover meaning, generalize, draw lessons from past experience, and solve problems. AI technologies are commonly used in healthcare, including areas such as critical care, feature machine learning, natural language processing, and computer vision.
If you’re curious about AI and its potential in the medical field, be sure to check out our blog for more articles to get a broader understanding of how AI is transforming the healthcare industry.
How can AI help healthcare providers?
The healthcare industry can benefit from the potential of artificial intelligence to support various functions, such as patient care and administrative duties. With the ability to mimic human cognitive functions, this technology brings advantages that surpass traditional analytics and other tools used for clinical decision-making. As a result, data quality improves, ensuring higher precision and accuracy, which can drive innovation in healthcare.
AI in intensive care medicine
The application of AI in critical care mainly involves disease diagnosis, prediction of disease progression (clinical deterioration), and characterization of specific disease phenotypes or endotypes in conditions such as sepsis, septic shock, and acute respiratory distress syndrome (ARDS).
The ICU provides an ideal environment for the implementation of AI technologies, and here is why:
Predictive analytics. ICU generates a large volume of patient data that can be used to train AI algorithms. Patient data collected in the ICU includes vital signs, laboratory results, imaging studies, and medication orders, among others. The large volume of data generated by daily patient care can be used to create AI models that can accurately predict clinical outcomes, such as the likelihood of clinical deterioration, and guide clinical decision-making.
Fast rates for prediction. Incomplete medical histories and large caseloads can lead to deadly human errors. However, AI technology is not affected by these variables and can identify patterns and trends in patient data that may not be immediately apparent to human clinicians. This can help healthcare professionals to make more accurate diagnoses, predict clinical outcomes, and tailor treatment plans to individual patients.
Workload demands. The critical care environment causes above-average burnout rates among ICU clinicians due to the stressful, demanding, and complex nature of their work. Burnout puts clinicians at risk of making medical errors, with nearly half of the workforce exhibiting symptoms. When surveyed, up to 45% of critical care physicians and 71% of pediatric critical care physicians suffer severe burnout, while 86% of critical care nurses experience at least one symptom of burnout. The cost of physician burnout alone is over $4.6 billion per year. To help alleviate these symptoms, critical care clinicians can use AI technology to manage demands being placed on them and improve their performance when caring for complex and high-acuity patients.
Optimizing patient care. The application of data science and AI techniques can improve the delivery of hospital care by utilizing complex data. A small controlled trial of 142 patients demonstrated that incorporation of AI technology into existing EHR-based sepsis identification systems was associated with decreased hospital length of stay and mortality reductions.
Our Healthcare Predictive Analytics Tool is a practical illustration of this AI-enabled transformation in care delivery. It empowers hospitals to predict admissions, surgeries, and potential health deterioration much earlier than traditional methods allow.
Another compelling example is our Automatic Reflex Diagnostics System, which demonstrates how AI can reduce critical diagnostic timescales in clinical settings. By processing reflex measurement data using advanced algorithms, the system provides physicians with a full picture of a patient’s health in just 15–20 minutes.
Machine Learning in ICU: Predicting, Identifying, and Optimizing Patient Care
Machine Learning (ML) is the dominant technique used for implementing AI systems. As technology continues to evolve, the possibilities for leveraging machine learning (ML) to revolutionize industries like healthcare become increasingly apparent. The automated processing of information through Machine Learning, and the possibility of rapid access to large volumes of data of a heterogeneous structure by means of Big Data Analysis, allow to improve the care processes and extract valuable knowledge from diverse and large datasets.
In this article, we will be focusing on the four main types of ML and their potential applications within the healthcare sector, particularly in intensive care units (ICUs). However, before diving into the specifics, it is important to have a foundational understanding of the main techniques used in ML. For a comprehensive overview of ML and its training processes, be sure to check out our article “Machine Learning: How to Train a Machine“.
Types of ML algorithms with use case examples
Classification of anomalies and false alarms, as well as patient state prediction in the ICU, are all important tasks that can be accomplished through supervised learning.
False alarms continue to be a problem whenever patients are monitored. In their publication, the research team used machine learning to reduce the incidence of false arrhythmia alarms. One of the methods for suppression of false alarms is composed of three main components: detecting the beats, determining the type of beats (for VF and VT alarms) and using an alarm-specific criteria to determine whether the alarm is false. The ML-supervised approach is used on the stage of determining the type of beats with the data annotated by human experts. This approach is often less strict than the definition of the alarm in order to prevent excessive false negatives and to account for possible missing beats.
Unsupervised learning can be used to automatically classify patients into groups, and to reduce the number of variables and the complexity of the models.
Medical images like CT scans or MRIs are common situations for a semi-supervised learning technique. A trained radiologist can label a small subset of scans for tumors or diseases. It would take up a lot of time to manually label all the scans — but the deep learning network can still benefit from the small proportion of labeled data and improve its accuracy in comparison to an unsupervised technique.
An example of reinforcement learning would be a system that learns and adjusts the optimal dosing of medication for a patient based on their physiological data and response to treatment, while minimizing the risk of adverse effects.
The algorithm of reinforcement learning can also be applied in ICU to address the extreme heterogeneity of septic shock, various underlying conditions, and different host-responses and then provide optimal individualized decision-making solutions for sepsis treatment.
Natural Language Processing (NLP)
Natural Language Processing is used to analyze and interpret human language and text data, such as unstructured clinical/nursing notes, diagnostic reports, physician’s letters, electronic health records (EHRs), and medical literature. NLP can be used to extract valuable insights from unstructured data, ensuring that each critical information has been uploaded to the patient’s health profile, thus improving the accuracy and efficiency of clinical documentation.
According to a recent study in the US, physicians spend an average of 16 minutes per patient using Electronic Health Records (EHR), which leads to both a reduction in patient care time and is a prominent cause of burnout and dissatisfaction among medical practitioners. Speech recognition systems with built-in NLP algorithms are being used to dictate patient notes. By shifting from handwritten notes to voice notes that NLP systems can analyze and add to EHR systems, healthcare professionals can improve record quality and reduce administrative burdens. This allows physicians to commit more time to the quality of care, ultimately enhancing patient outcomes.
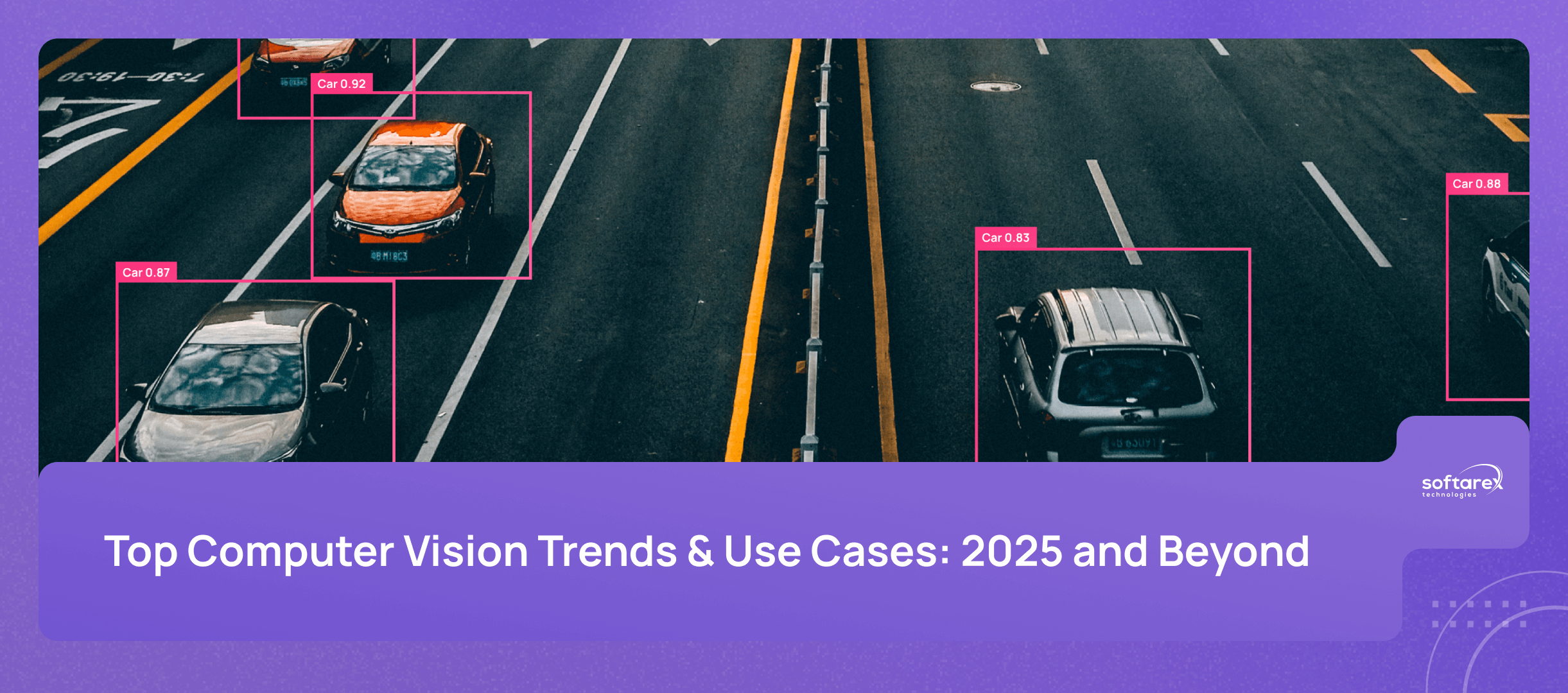
Computer Vision
Computer vision is used to analyze and interpret medical images, such as X-rays, MRIs, and CT scans. This field of AI can help healthcare providers detect abnormalities and diagnose conditions, as well as track disease progression and treatment effectiveness.
In Conclusion
Artificial intelligence has immense potential in the ICU and is a valuable technology for the healthcare industry. It enables personalized treatment plans for individual patients, provides accurate and precise data, and improves the diagnosis and treatment processes, ultimately leading to better patient outcomes. As new developments in AI emerge, the potential for even more benefits is promising.
If your healthcare organization is considering implementing AI in the ICU, our technical experts can assist with custom software development to design and implement a tailored solution. Schedule an online consultation with us today to learn more.